About Tuberculosis (TB)
-
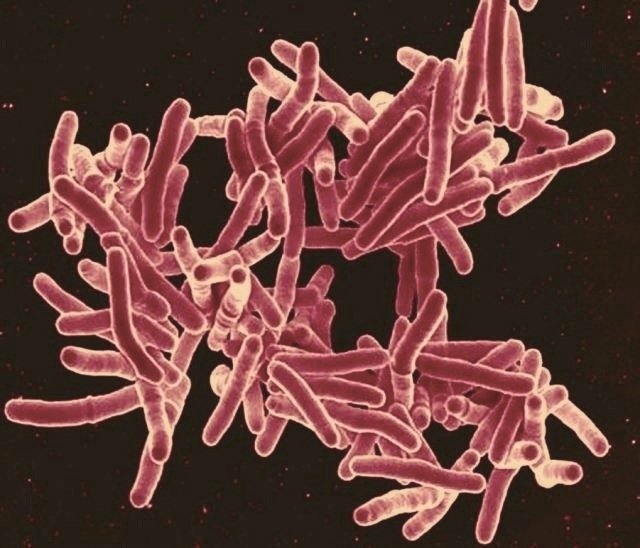
Tuberculosis is an infectious disease caused by a bacteria that can affect humans.
The disease most commonly affects the lungs but can affect other organs e.g. spine, abdomen, glands etc.
TB can either be active disease, where you are unwell and might have symptoms.
Or you could have latent TB infection, which is when your immune system has met the bacteria but you do not have any symptoms. This latent bacteria, could wake up and you could go on to develop active TB disease, especially if your immune system is weakened.
-
TB is spread when people with active TB disease have the bacteria in their lungs. When they cough, sneeze, talk, or breathe, the bacteria travel through the air in droplets which can be inhaled by others, leading to them become infected.
-
Symptoms of active TB disease, especially when it affects the lungs, include:
A persistent cough, lasting more than 2–3 weeks (this could be productive or dry)
Coughing up blood
Chest pain, especially when breathing or coughing
Unexplained weight loss
Fever and drenching night sweats
Fatigue and weakness
Loss of appetite
Swelling of the glands
People with latent TB infection won’t have any symptoms or be able to pass the bacteria to others. However, the bacteria remain in their body and could become active later. This means it is always worth testing someone who has potentially been exposed to the bacteria.
These symptoms are not definitive. Some people experience different symptoms. If you have a concern about TB exposure, a known TB contact or come from a country where there are higher rates of TB disease, it’s important to think TB!
If you have symptoms and are concerned contact your health provider.
-
Active TB disease is usually diagnosed through a combination of:
Symptoms
Radiological scans (Chest X-rays, CT scans etc.)
Laboratory tests (e.g sputum testing)
TB disease can be difficult to get a definitive diagnosis, so the diagnosis pathway might differ.
Latent TB infection is usually diagnosed if:
Someone is suspected of being a close contact with somebody with active TB disease, comes from a country with high rates of TB or other risk factors are identified.
They have no symptoms.
They have a normal radiological scan (Chest X-rays, CT scans etc.).
They have a positive blood or skin test.
Track and trace programmes, such as contact tracing for TB disease, also play a vital role in identifying and supporting people who may have been exposed. This helps to prevent the spread of infection, protecting families, communities, and those at higher risk. Active TB can then be treated early or preventative treatment can be offered if someone has latent TB infection.
-
TB is treatable, curable, and TB treatment is free worldwide!
Active TB disease treatment usually lasts for 6 months, with a course of oral antibiotics. Depending on where in the body the active disease is, treatment may last longer. For example up to 12 months for spinal TB disease.
For the majority of the time, TB treatment can be managed as an outpatient, so you wouldn’t need to be admitted to hospital unless you were extremely unwell.
Your medical care team or TB nurses would support you through your treatment journey, explaining medications and side effects with you.
It is important to take TB medications every day and complete the course of treatment as prescribed, even if symptoms improve early. This is to reduce the risk of bacteria becoming resistant to the antibiotic drugs (MDR-TB and XDR-TB).
Drug-resistant TB requires longer, more complex treatment, which often involves more medications, more adverse, longer term side effects, and poorer outcomes.
-
Early detection and treatment:
prevents you from becoming seriously unwell.
can help prevent serious health complications.
reduces the risk of spreading TB to others
improves outcomes and treatment is better tolerated when started early.
Treating latent TB infection:
can prevent it from becoming active TB disease, which can help protect your loved ones.
involves fewer medications and is better tolerated.
-
What is MDR-TB?
MDR-TB stands for Multidrug-Resistant Tuberculosis.
It doesn’t respond to (is resistant to) the two main TB medicines Isoniazid and Rifampicin.
This makes it much harder to treat than regular TB disease, and treatment takes longer, often with more side effects.
What is XDR-TB?
XDR-TB stands for Extensively Drug-Resistant Tuberculosis.
It’s a rare but an even more serious form of drug-resistant TB. XDR-TB is resistant to:Isoniazid and Rifampicin (the two main TB drugs)
Second line antibiotics (such as fluoroquinolones)
This makes XDR-TB extremely difficult to treat and requires highly specialised care.
Is MDR/XDR-TB curable?
Yes, but it requires longer and more complex treatment, often involving different medications over 18–24 months. Early diagnosis and expert care are essential for better outcomes.
Why are we so concerned about drug-resistant TB?
Drug-resistant TB is hard to treat and patients have poorer outcomes. Early intervention is very important.
-
Yes!
TB disease remains one of the deadliest infectious diseases in the world.
In 2023, it caused an estimated 1.25 million deaths, surpassing even COVID‑19 as the leading cause of death from a single infectious agent.
TB disease is a problem globally and here in the UK, where rates of TB disease are on the rise.
1 in 4 people (a quarter of the world) have the latent TB infection and there is a 5-15% chance that this could become active TB disease in their lifetime. This shows the importance of early detection and preventative treatment.
-
Who is most affected by TB?
Anyone! TB does not differentiate, it does not care whether you’re rich or poor, it does not care where you come from and therefore anybody can be at risk of having latent TB infection or developing active TB disease.
There are some people who might be at slightly more risk, for example those:
living in overcrowded or poorly ventilated housing.
experiencing malnutrition or homelessness.
living with HIV/AIDS.
are in contact with health systems that are under-resourced.
have other health conditions or risk factors.
These factors make TB disease not just a medical issue, but also a social justice issue!
-
Regardless of whether you are undocumented or have insecure immigration status you will still received diagnosis, treatment and care for your TB disease.
TB care is always confidential.
Our primary goal is to support you and your health regardless of your background.
Excluding people from care doesn't just put them at risk, it puts public health at risk too.
Tackling it effectively means ensuring everyone has access to care.
No one should be afraid to seek care!
-
Yes!
In the UK, TB treatment is free of charge for everyone.
Learn more about Tuberculosis from these other great resources
-

World Health Organization
-

National Health Service UK
-

UK Government and UK Health Security Agency
-

Results UK
-

Médecins Sans Frontièrs (MSF)
-

Stop TB Partnership
-

TB Alert
